Natural selection in human eggs and embryos in the first days of development is very strict.
On average only 5% of human naturally ovulated eggs result in a baby. Only half of fertilized eggs become viable embryos on day 5.
In IVF there will be always more eggs collected than eggs which will successfully get fertilized (merged with a sperm), and not all of those eggs which get successfully fertilized will cleave (continue to divide). There will always be more viable embryos on the day after egg retrieval than there will be on day 3 and some embryos which were viable on day 3 will have already stopped growing by day 5 – this is perfectly normal. In our experience and in fertility literature on average half of fertilized eggs become viable embryos on day 5, in egg and embryo donation programmes.
Paternal Genes only switch on in the embryo after day 3. It was found in many studies that until day 3 (inclusively) embryo development is mostly controlled by the genes of the egg. Even an unfertilized egg can go ahead cleaving for up to 3-4 days! Only after day 3 do the paternal genes switch on and begin to influence the development of the embryo.
Growing embryos to day 5 is crucial. This is why it is so important to grow embryos for 5 days; to get as much possible information about their preimplantation development, so as in order to be able to choose the best embryo for transfer and which will give you the maximal chance of becoming pregnant.
How is the choice of the best embryo done under the microscope?
 Choosing the best embryo for transfer under the microscope: Many cells in the inner and outer cell mass means a higher implantation rate.
Choosing the best embryo for transfer under the microscope: Many cells in the inner and outer cell mass means a higher implantation rate.
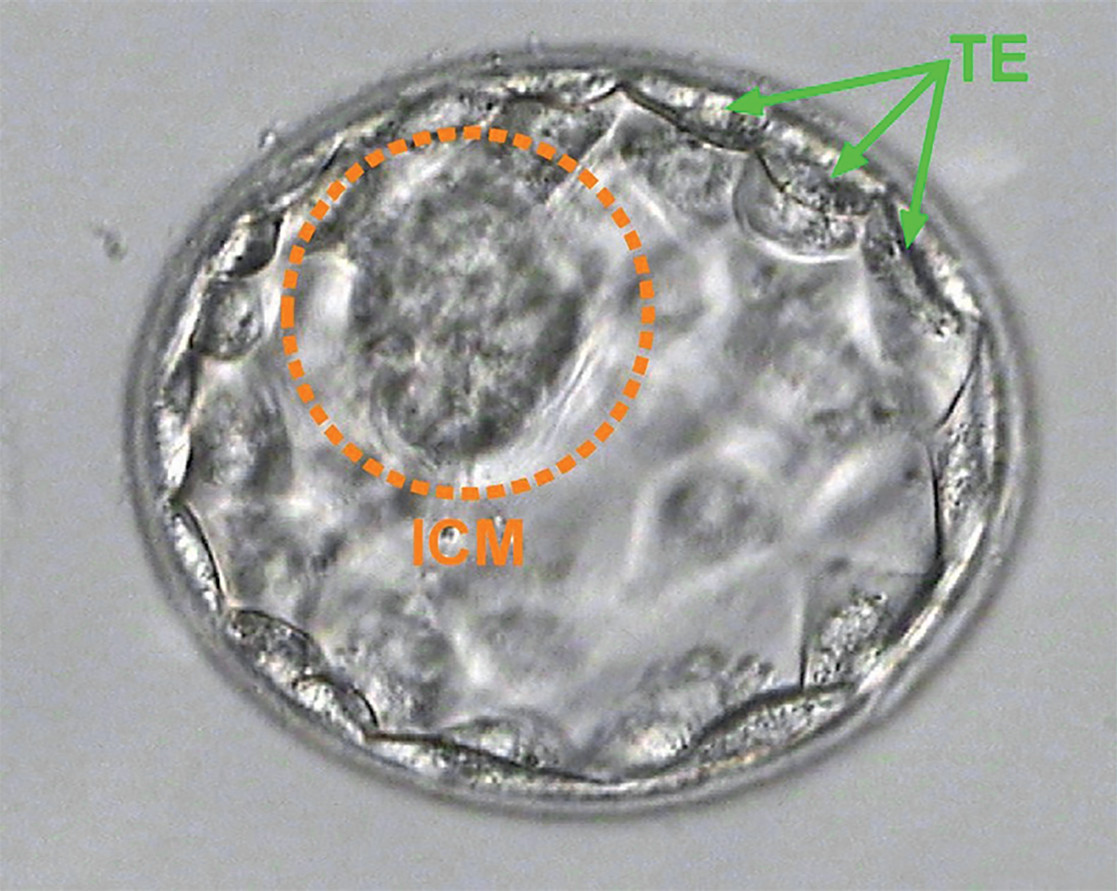
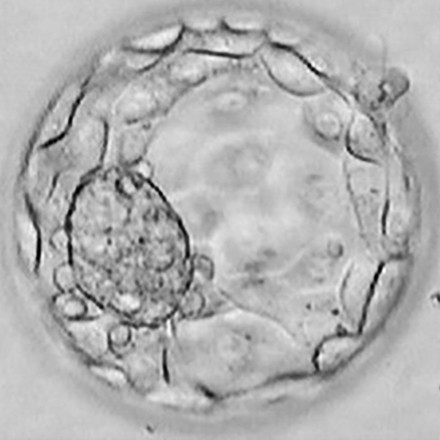
We select the best embryo for the embryo transfer on day 5 after the egg retrieval, a 5 day old embryo is called a blastocyst. This is the first stage in embryonic development, which has more than one type of cell. A blastocyst looks like a sphere with a bunch of cells glued to it from inner side. The cells forming the sphere are called “outer cell mass” or “trophectoderm” and will form the placenta and fetal sack. The bunch of cells on the inner side of the sphere is called “inner” cell mass and will hopefully be the body of the baby in the future.
After many years of experience, certain patterns of embryonic ‘looks’ under a microscope on day 5 were seen to correlate with the level of implantation rates achieved through transfer of these particular embryos. Not surprisingly, it was shown that if there were very many cells in the inner and outer cell mass, the success rates were high, and vice versa – if there were too little cells – the chance of implantation was very low.
Blastocyst grading according to their looks aims to choose the embryo for transfer which is the most likely to achieve implantation.
This is the short summary of ‘Gardner classification’ which is often used for blastocyst grading and subsequent choosing of embryos to transfer.
The first letter standing after the abbreviation “BL” for blastocyst, relates to the inner cell mass; the second letter relates to the outer cell mass.
A — very many cells
B — many cells
C — low number of cells
D — very low number of cells
For example:
A blastocyst ‘BL AA’ has very many cells in inner and outer cell mass.
A blastocyst BLAB has very many cells in the inner cell mass and many cells in outer cell mass.
BL AA, AB or BA have very high chance to attach in the uterus. This is why they are called, or referred to as ‘superior quality blastocysts’, ‘superior morphology blastocyst’ or ‘excellent blastocyst’.
 BL AA
BL AA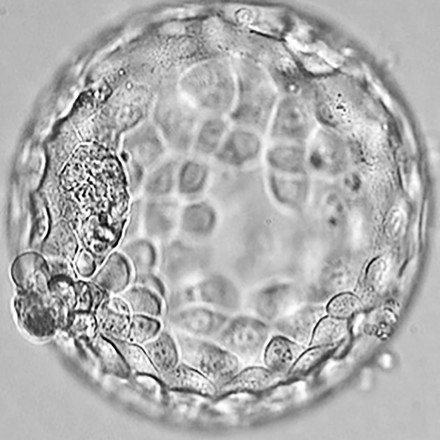 BL BA
BL BA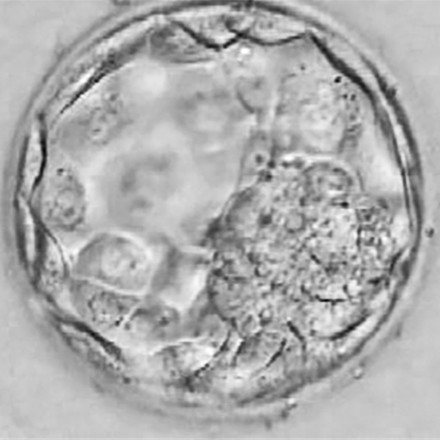 BL AB
BL AB BL BB
BL BB BL AC
BL AC BL BC
BL BC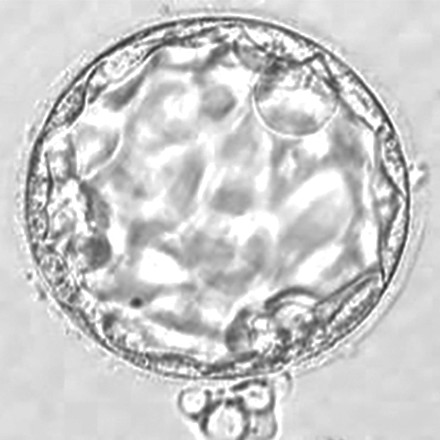 BL CB
BL CB BL CC
BL CCThis grading/description is based only on the looks of the embryo under microscope und correlates with nothing else, but probability of this embryo to attach in the uterus. This superior quality has nothing to do with general health, success in school, or quality of life! We will never forget a lovely couple from Germany that commented that their son Mathias was not of superior quality at transfer ‘but look at him now at the age of 3, tall, smart and cleverer than any other child in their kindergarten group’
If you are lucky to have a superior morphology blastocyst in your embryo pool we recommend transferring this embryo. The clinical pregnancy rates with one superior quality fresh blastocyst chosen by morphology are 54% and 52% with frozen. Transferring two top morphology embryos will not double the chances, but will significantly increase the risk of having multiple pregnancy. After transfer of 2 superior quality blastocysts 70% of patients become pregnant and more than half of these pregnant with twins.
Multiple pregnancy is known to have 5-6 times higher incidence of complications in the mother during pregnancy and birth and the children born to them, than in a singleton pregnancy; most problems are attributed to very early birth and very low birth weight.
If there are only blastocysts of BB or BC quality available in embryo group, we will discuss an opportunity of transferring two embryos to keep chances high. If transferring 2 BB/BC blastocysts the chances of getting pregnant will still be 55-60%, but the incidence of twin pregnancy will be less than 20%.
Our main goal is to always keep chances for a baby high and the risks low. We always remain individual at every stage of treatment, from the very beginning at donor choice to choosing the number of embryos for chances; our main goal is to always keep chances for a baby high and the risks low.
Blastocysts are also graded via numbers from 1 till 6
 BL1
BL1 BL2
BL2 BL3
BL3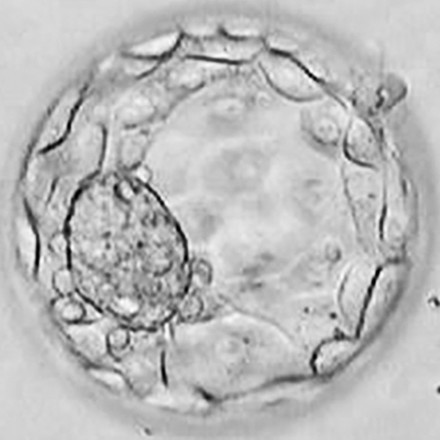 BL4
BL4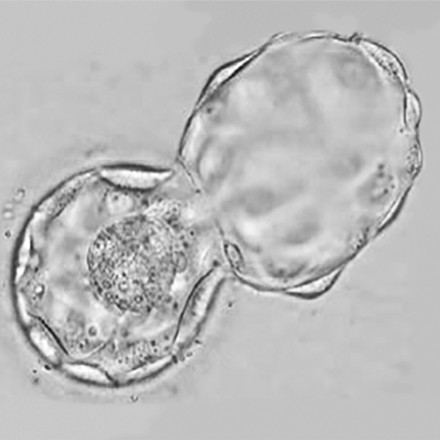 BL5
BL5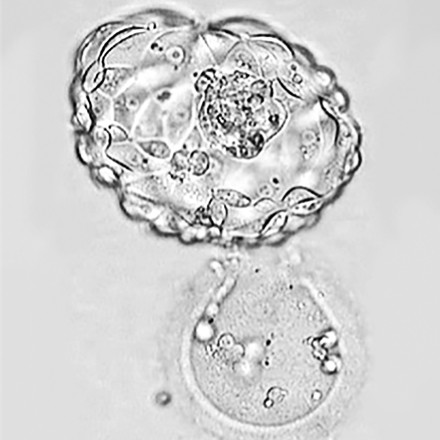 BL6
BL6BL1 — just turned into blastocyst form, the previous morula stage.
BL2-3 — a blastocyst in the process of expanding
BL4 — well expanded blastocyst
BL5 — a blastocyst in the process of hatching
BL6 — completely hatched blastocyst ready for implantation
Why can we not culture longer than 5 days?
In the end of day 5 leading into day 6 an embryo comes out of the egg membrane. Receptors on the surface of the outer cell mass become open for recognition process between them and receptors on the endometrial cells in the uterus. The embryo is ready for implantation and needs to be transferred to the uterus.
So day 5 is the last day we have opportunity to evaluate the embryo outside the body.
Are all embryos which are good looking on day 5 capable of developing to a live birth?
A wise man once said: “All that glitters is not gold”. Surprisingly, not all the good looking embryos are as promising as they may look. Some embryos which are good looking on day 5, but have internal problems will soon stop development and result in negative pregnancy test, or early miscarriage. These internal problems are most frequently caused by abnormal chromosome number in the embryo.
Normal human cells have 23 pairs of chromosomes. Having one, or several, chromosomes extra, or less has almost always a lethal effect on the embryo either in preimplantation stage or in early pregnancy. However, there are exceptions to this rule such as Trisomy 21 which continues development until live birth, but results in the birth of a baby with Downs Syndrome.
Two sibling embryos one with normal chromosome count and one with abnormal chromosome count may look under the microscope absolutely similar superior morphology blastocysts.
So what is known?
- Humans produce a large percentage of eggs and embryos with abnormal chromosome count (aneuploidy)
- Aneuploidy is almost always lethal for embryo (the main reason of implantation failure, or early miscarriage as nature recognizes these chromosome mistakes and stops them)
- Influence of aneuploidy on embryonic ‘looks’ on day 5 is minimal (two sibling embryos one with normal chromosome count and one with abnormal chromosome count may look under the microscope absolutely similar superior morphology blastocysts of AA quality!)
Is there any way to identify which of the good looking embryos has abnormal chromosome count and will stop development several days, or weeks after the embryo transfer? It would be helpful to exclude this embryo from usage and save time and hope for the patient!
Yes, such a method exists. It is called PGS — preimplantation genetic screening.
20-30% of good looking donor egg embryos have abnormal chromosome number and are incapable of creating a baby.
In our experience and literary data the percentage of aneuploid embryos in your embryo pool correlates with the age of an egg. In 35 year old women half of blastocysts are abnormal, in 40 year old women 70% of blastocysts are abnormal. In other words the higher the age the higher the aneuploidy rates.
| Egg Donors | < 35 years | 35—37 years | 38—40 years | 41—42 years | > 42 years |
|
65% |
56% |
46% |
33% |
19% |
13% |
S. Munne et al. Blastocysts needed to transfer at least one euploid embryo: data from 10,852 pre-implantation genetic screening (PGS) cycles. Fertility Sterility September 2015 Volume 104, Issue 3, Supplement, Pages e13–e14
Surprisingly even in blastocysts created from egg donor eggs 30% of blastocysts are abnormal!
Hence if choice is done only on the basis of morphology on day 5 a good looking embryo, but with abnormal chromosome count may be chosen for transfer, with a risk of 70% in a 40 year old patient using own eggs, or with a risk of 20-30% in an egg donor cycle.
So an average egg donation protocol in our experience and knowledge would typically look like the following:
- 14 eggs retrieved
- 12 mature, 10 fertilized normally,
- 5 viable embryos to expect on day 5.
- 1-2 of them have abnormal chromosome count,
- 3-4 – have normal chromosome count.
So what are the benefits of PGS in donor egg/embryo cycles?
What are the benefits of PGS and why do our patients choose to use it?
- PGS does not make your embryos better! PGS ensures the selection of embryos with normal chromosome set from those available.
- PGS increase implantation rates and live birth rates per embryo transfer, but not per egg retrieval.
- PGS reduces time to pregnancy and live birth
- Reduces miscarriage rates
- Helps avoid freezing and storage of abnormal embryos
- Reduces risk of Down syndrome
How is a sample for testing taken from an embryo?
How is PGS carried out — will it harm my baby?
To be able to check the embryo’s chromosome count at least one cell from the embryo is needed. This cell can be taken from the embryo via biopsy. The first and the last stage in which this manipulation is harmless for pre-implantation embryo is at blastocyst stage (5 day old embryo). Biopsy in the earlier stages was proven to decrease implantation rates due to significant influence on amount of cells left in the embryo. Biopsy on day 5 was shown to have no negative impact on the embryo: implantation rates were the same in the day 5 biopsy group Vs no biopsy. It is confirmed that biopsy on day 5 in an experienced lab does not harm the embryo.
The embryo needs to be frozen via vitrification after biopsy so the time stops for the embryo and professionals can use this time to receive the results of the genetic testing. Vitrification of blastocysts does not have negative impact on the embryo, or the success rate. Transfer of one non tested fresh embryo results in a 54% clinical pregnancy rate, transfer of one non tested frozen embryo results in a 52% clinical pregnancy rate and one PGS tested, frozen embryo, normal for 23 chromosome pairs results in a clinical pregnancy rate of 60%
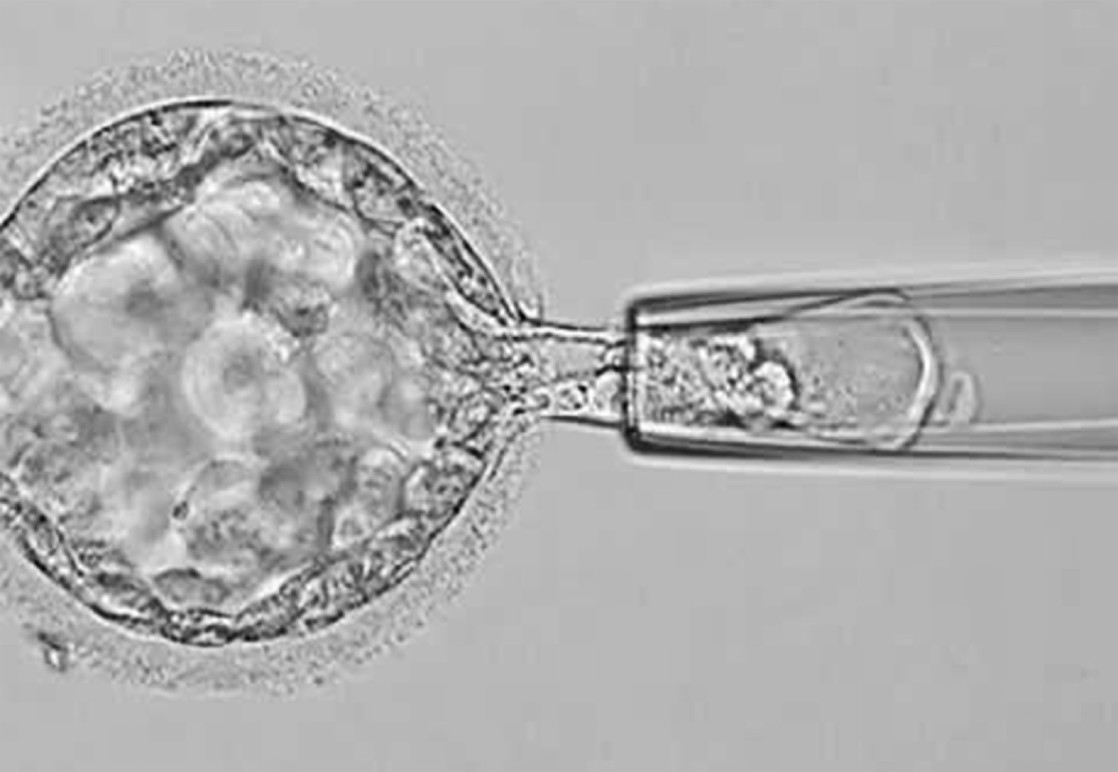 This is the way the biopsy is carried out. As you see a small cell sample is taken from the outer cell mass – the future placenta. No biopsy is taken form the inner cell mass- the future embryonic body.
This is the way the biopsy is carried out. As you see a small cell sample is taken from the outer cell mass – the future placenta. No biopsy is taken form the inner cell mass- the future embryonic body.
Manipulation in the lab on later stage embryo is not possible because an embryo needs to be returned in the uterus at latest on day 6 due to its needs to attach in the uterus.
How does the process of PGS work and how does the selection of embryo for transfer done on the basis of both good morphology and normal chromosome benefit the recipient?
Embryos are grown 5 days
↓
Biopsy of placenta cells is performed on all A and B grade blastocysts
↓
All blastocysts are immediately frozen after the biopsy
↓
DNA is extracted from the biopsied sample and amplified (to have more copies of DNA for testing)
↓
Chromosomes are counted via a-CGH method (takes several days –several weeks)
↓
Results from a-CGH are correlated with corresponding embryos and embryos with abnormal chromosome count are discarded
↓
The best morphology embryo is chosen from those which have normal chromosome count, is then thawed and used for the embryo transfer
↓
All the remaining embryos with normal chromosome count remain the property of the patient, stay in the freezer and can be used for another try if necessary, or for a sibling several years later.
What are the success rates?
With one embryo chosen by morphology and genetics implantation rates are 60%.
In our egg and embryo donation program while with one frozen embryo chosen on morphologic criteria only, implantation rates are 52%, with one embryo chosen by morphology and genetics implantation rates are 60%.
Good morphology correlates with embryonic chance to attach.
Normal chromosome count correlates with embryonic capability to proceed to live birth.
The highest live birth rate per each embryo use for transfer is achieved if embryo is chosen on the basis of both, the morphology and the genetics.